Should every diabetes service have a psychologist?

Introduction
As a clinical psychologist who has worked in diabetes for many years, I have observed that there has always been a core of practitioners with strong interests in the psychosocial aspects of the condition, and a strong commitment to disseminating their skills. Despite this, it is common for the nonphysical aspects of diabetes to be neglected in busy day-to-day practice in adult teams. This is not surprising, as most diabetes health care professionals (HCPs) have been trained in the biomedical model, with psychological process discussed separately rather than integrated within every topic.
My purpose in this paper is to outline the benefit of having a psychologist or other mental health care professional (MHCP) in an adult multidisciplinary diabetes team (from here referred to as the diabetes team). Most paediatric teams have a MHCP in the team or within the hospital, however, most adult diabetes teams do not have a psychologist within their system. I will draw from my experience working both as part of and external to diabetes teams. I will also demonstrate that the role of a psychologist goes beyond just working with people who are going through high levels of emotional distress or who have a psychological disorder. MHCPs can and should be involved in a range of areas including: consulting to the team, assisting with goal setting, assisting with lifestyle change, consulting regarding behaviour modification techniques, assisting with clarifying targets for glycaemic management, developing and maintaining programs to foster social cohesion and support amongst similar cohorts of people with diabetes, and evaluating programs that are developed. Clinical and health psychologists are uniquely placed to carry out all of these tasks.
The need for a psychological perspective
It has been recognised for many years that a reliance on the biomedical model (a focus on physiological processes to the exclusion of psychological, behavioural or social processes1) is not sufficient in the management of diabetes. Joan Williams Hoover2 famously developed the concept of Diabetes Burnout, noting the large personal effort and large number of decisions a person with diabetes has to make each day – this is in addition to the frustration and sense of failure often generated by the unpredictability of diabetes. Individuals with diabetes are at increased risk for depression and diabetes distress, and both are linked to decrements in self-management, quality of life, and diabetes-related outcomes.3, 4 In the second Diabetes Attitudes, Wishes and Needs (DAWN2) study,5 significant diabetes distress was reported by 45% of the participants, but only 24% reported that their HCPs had asked how diabetes affected their lives.
Historically, numerous practitioners have been at the forefront of advocating for better communication, empowerment, person-centred care, and recognition of the emotional burden of diabetes.6, 7, 8 The creation of the Australian Centre for Behavioural Research in Diabetes (dedicated to investigating the behavioural, psychological and social aspects of people living with diabetes) in 2010 has been a boon to bringing attention to psychosocial aspects of diabetes. The DAWN1 and DAWN2 studies have increased understanding of the key facilitators and barriers to person-centred care, and helped identify successes, wishes, needs, preferences, and priorities among key stakeholders in diabetes.9, 10 Guidelines for diabetes management in Australia and worldwide all note the importance of access to MHCPs, and that all members of a diabetes team must pay attention to emotional needs and screen for emotional ill health.11, 12, 13 Integrating this information, the publication in Australia of the Diabetes and Emotional Health Handbook14 has allowed clinicians easy access to essential psychosocial information and concepts. This excellent work puts emotional health at the forefront of diabetes management. It gives clinicians an overview of emotional issues likely to be faced by people with diabetes, and provides professionals with information to assist referral to a MHCP should the individual with diabetes be experiencing levels of emotional distress deemed to require treatment.
This push to upskill diabetes HCPs is important and necessary. Diabetes distress is a common part of the diabetes journey, usually waxing and waning over time. Diabetes HCPs need the skills to notice and deal with these changes confidently, competently, and empathically. Additionally, they require excellent skills in recognising and referring people with varied psychological disorders such as depression, anxiety, eating or adjustment disorders, which are common, and known to decrease self-care behaviours and increase HbA1c levels.15 However, having psychologically aware HCPs on a team is not equivalent to having a MHCP in the team. A MHCP is able to perform specialist functions that other HCPs are not trained for. Team members should be able to refer easily to a MHCP for more complex psychological care that remains within the team. This is similar to a diabetes educator addressing basic nutrition matters themselves, but referring to a dietitian for individualised medical nutrition therapy.
Young-Hyman and colleagues12 provide a model of the role of a “behavioural or mental health provider” in a diabetes team at different phases of a person’s diabetes journey (see figure 1). They emphasise that psychosocial and emotional issues occur along a continuum of severity, and that all team members (including the MHCP) are responsible for helping the person with diabetes to cope when symptoms are at a nonclinical level. In this model, the MHCP potentially has involvement with people with diabetes at any stage of their functioning, not only when symptoms of psychological disorder are present.
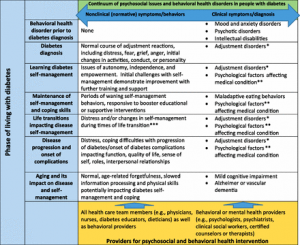
Figure 1. From Young-Hyman et al (2016)
Benefits of embedding a mental health care professional within a diabetes team
Treating psychological disorder within the diabetes care context
Having a MHCP embedded in the diabetes team can prove valuable should a person with diabetes develop symptoms of psychological disorder that require a mental health referral. Possible problems include those directly related to diabetes, such as severe anxiety about hypoglycaemia, fear of developing complications, adjustment difficulties to a new diagnosis, or disordered eating or insulin behaviour. They can also include problems minimally related or completely unrelated to diabetes. Heindrieckx and colleagues14 note that people with diabetes often prefer to receive psychological assistance within the context of their diabetes treatment. My own experience suggests a higher uptake of psychology services when I am working in a team than as an external practitioner. This may be because the MHCP is already a familiar face, is convenient to access, and is better known to the referrer and so more likely to be endorsed wholeheartedly by them. Additionally, if the person being referred is nervous, it is often possible to organise a quick meeting on the day of the referral, which can remove a great deal of fear and uncertainty (and stigma) about the MHCP.
According to the American Diabetes Association,13 the integration of mental and physical health care can improve outcomes. They note research suggesting that when a person is in psychological therapy, the mental health provider should be incorporated into the diabetes treatment team.16 Combined treatment of depression and diabetes self-management results in improvement in both depression and diabetes outcomes, while treatment of the depression alone alleviates depression but does not usually result in much improvement in diabetes outcomes.17
Having a MHCP on a diabetes team is not, however, solely about facilitating referrals for mental health disorders or dealing with diabetes distress (although both are important functions!). There are numerous ways in which a MHCP can add value to a diabetes team and result in better outcomes for improved quality of life and better glycemic management. Although the needs of those with type 1 diabetes (T1D) and type 2 diabetes (T2D) are often different, there is overlap, and the following areas refer broadly to both conditions.
Improving communication and consistency of treatment
A MHCP embedded in a diabetes team increases the ability of all stakeholders (person with diabetes and all staff) to liaise productively and easily, thereby easily working toward shared outcomes. The MHCP can be present during appointments between the person with diabetes and other staff members. There is opportunity for multidisciplinary meetings, as well as spontaneous communication regarding referrals, assessment outcomes, treatment goals and other important aspects of care. Additionally, all team members have access to the same medical record, which assists communication and consistency. This makes it much easier to integrate physical and psychological aspects of treatment, and is very different to relying on an occasional letter from an off-site care provider.
Tailoring strategies for optimal glycaemic management
MHCPs can help people with diabetes achieve optimal glycaemic management, regardless of whether or not they experience a psychological disorder. This was also recognised by the Diabetes Control and Complications Trial Research Group18 who included psychologists on the team to assist with optimal glycemic management. The National evidence‐based clinical care guidelines for type 1 diabetes in children, adolescents and adults11 recommend individualising strategies of intensive glycemic management as much as is practical. Psychologists are well placed to work with individuals to design workable and sustainable targets, and overcome barriers that arise. They can assist with clarifying a person’s priorities and values, levels of confidence or self-efficacy, level of social and family support, and the overall burden of treatment.12
Behaviour modification and lifestyle change
Psychologists have been key developers of behavioural lifestyle programs, which are the first line of treatment for T2D (e.g. the LOOK AHEAD programme19) and also important for some people with T1D. Although these resource intensive “gold standard” programs may be outside the reach of many diabetes centres, there are undoubtedly many achievable and efficacious behavioural interventions that are not currently a part of routine care in many diabetes centres. The presence of a psychologist would allow each centre to optimise its behavioural change programs within available resources. Behaviour modification techniques such as stimulus control, urge surfing, distress tolerance, self-soothing, relapse prevention and coping with self-defeating thoughts can all be included within group programs, and the inclusion of a psychotherapy component in a comprehensive diabetes and obesity program potentially increases the amount of weight lost.20
Improving uptake and consistent use of new technologies
The huge and beneficial advances in technology of the last decades can sometimes lead to neglect of psychosocial issues. As the technology becomes more sophisticated, there can be an assumption that this in itself will lead to better glycaemic management. However, not everyone can benefit equally from newer technologies. At present, optimal use of technology requires a person to have good executive functioning and reasonable levels of psychological health. This means that people can struggle to use the technology they are provided with, or find the constant effort needed overwhelming, leading to giving up. Psychologists are well placed to help people adjust to the demands of technology. This includes both adapting to new technologies, and also continuing with its consistent use.21
Improving quality of life
In addition to being involved in more traditional behaviour modification programs, MHCPs also have a role to play in developing creative programs that can boost self-care, quality of life, and glycaemic management among people with diabetes. Examples of this include stress management or mindfulness interventions for diabetes, emotional eating programs, interventions to increase family support, or interventions to increase peer support.22
Training, supervising and consulting to other team members
Having a MHCP on a diabetes team means that the team can frequently benefit from their psychological expertise. HCPs cite lack of skills, confidence, time, and limited access to practical resources as common barriers to engaging with the psychosocial needs of people with diabetes.23 The MHCP is able to provide ongoing support, as well as more formal inservices and training on a variety of psychological topics and skills. This can help to build confidence and encourage team members to try various new strategies. Additionally, the MHCP can function as a consultant or provide supervision for complex cases. Psychologists also have skills for evaluating programs, and this can be extremely useful in a busy team.
Conclusion
According to the ADA’s 2020 Standards of Care in Diabetes, “Effective behavior management and psychological well-being are foundational to achieving treatment goals for people with diabetes”.13 It follows that all HCPs on a diabetes team should be literate in the psychological needs of people with diabetes. However this alone is often not sufficient. It is essential that, when required, both staff and people with diabetes have access to the specialist services of a MHCP. Locating the MHCP within the team reduces obstacles such as access, stigma, communication, and location, and increases the likelihood of people with diabetes receiving treatment. It also makes it possible for the MHCP to assist people experiencing everyday difficulties and frustrations (such as behavioural setbacks or difficulty with changing habits) but who have no significant diabetes distress or mental health disorder. Although this latter group can often benefit substantially by learning to apply psychological tools to manage their struggles, they are unlikely to gain access to a MHCP who is not part of the diabetes team. In my experience, people with diabetes greatly appreciate the presence of a MHCP within a team, as they can easily contact a familiar person with expertise in both psychology and diabetes.
As noted by Bateman,24 easy access to a psychologist is seen as essential in some healthcare settings (e.g., cancer or HIV diagnoses). Unfortunately, there is still a long way to go in diabetes care before this can occur. Although it is neither necessary nor realistic for everyone with diabetes to see a psychologist, the psychological skills and health of people with diabetes are clearly intertwined with optimal self-management of the condition. It is therefore my strong belief that a psychologist should be considered as an integral member of a multidisciplinary diabetes team.
References
1.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977 Apr;196(4286):129â36. https://doi.org/10.1126/science.847460PMID:847460
2.Hoover JW. Patient burnout, and other reasons for noncompliance. Diabetes Educ. 1983;9(3):41â3. https://doi.org/10.1177/014572178300900308PMID:6557914
3.Holt RI, de Groot M, Lucki I, Hunter CM, Sartorius N, Golden SH. (2014) NIDDK International Conference Report on Diabetes and Depression: Current understanding and future directions. Diabetes Care.2014 Aug;37(8):2067-2077. https://doi.org/10.2337/dc13-2134 PMID:25061135
4.Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014 Jul;31(7):764â72. https://doi.org/10.1111/dme.12428PMID:24606397
5.Funnell MM, Bootle S, Stuckey HL. The diabetes attitudes, wishes and needs second study. Clin Diabetes. 2015 Jan;33(1):32â6. https://doi.org/10.2337/diaclin.33.1.32PMID:25653471
6.Tupling H, Webb K, Harris G, Sulway M. Youâve got to get through the outside layer: A handbook for health educators using diabetes as a model. Sydney (AU): Diabetes Education & Assessment Programme Royal North Shore Hospital; 1981.
7.Gonder-Frederick LA, Cox DJ, Ritterband LM. Diabetes and behavioral medicine: the second decade. J Consult Clin Psychol. 2002 Jun;70(3):611â25. https://doi.org/10.1037/0022-006X.70.3.611PMID:12090372
8.Delamater AM, Jacobson AM, Anderson B, et al.; Psychosocial Therapies Working Group. Psychosocial therapies in diabetes: report of the Psychosocial Therapies Working Group. Diabetes Care. 2001 Jul;24(7):1286â92. https://doi.org/10.2337/diacare.24.7.1286PMID:11423517
9.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005 Oct;22(10):1379â85. https://doi.org/10.1111/j.1464-5491.2005.01644.xPMID:16176200
10.Peyrot M, Burns KK, Davies M, et al. Diabetes Attitudes Wishes and Needs 2 (DAWN2): a multinational, multi-stakeholder study of psychosocial issues in diabetes and person-centred diabetes care. Diabetes Res Clin Pract. 2013 Feb;99(2):174â84. https://doi.org/10.1016/j.diabres.2012.11.016PMID:23273515
11.Craig ME, Twigg SM, Donaghue KC, et al, for the Australian Type 1 Diabetes Guidelines Expert Advisory Group. Draft National evidenceâbased clinical care guidelines for type 1 diabetes in children, adolescents and adults. Canberra (AU): Australian Government Department of Health and Ageing; 2011. 257 p.
12.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial Care for People with Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016 Dec;39(12):2126â40. https://doi.org/10.2337/dc16-2053PMID:27879358
13.American Diabetes Association. Standards of Medical Care in Diabetes 2020. Diabetes Care. 2020 Jan;43(Supplement 1).
14.Hendrieckx C, Halliday JA, Beeney LJ, Speight J. Diabetes and Emotional Health. A handbook for health professionals supporting adults with type 1 or type 2 diabetes for Australian Centre for Behavioural Research in Diabetes. Melbourne (AU): Australian Centre for Behavioural Research in Diabetes; 2016. 183 p.
15.de Groot M, Golden SH, Wagner J. Psychological conditions in adults with diabetes. Am Psychol. 2016 Oct;71(7):552â62. https://doi.org/10.1037/a0040408PMID:27690484
16.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010 Dec;363(27):2611-20. https://doi.org/10.1056/NEJMoa1003955PMID:21190455
17.van der Feltz-Cornelis CM, Nuyen J, Stoop C, et al. Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2010 Jul-Aug;32(4):380â95. https://doi.org/10.1016/j.genhosppsych.2010.03.011PMID:20633742
18.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993 Sep;329(14):977â86. https://doi.org/10.1056/NEJM199309303291401PMID:8366922
19.Look AHEAD Research Group, Wadden TA, West DS, et al.; Look AHEAD Research Group. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring). 2006 May;14(5):737â52. https://doi.org/10.1038/oby.2006.84PMID:16855180
20.Foster D, Sanchez-Collins S, Cheskin LJ. Multidisciplinary Team-Based Obesity Treatment in Patients with Diabetes: Current Practices and the State of the Science. Diabetes Spectr. 2017 Nov;30(4):244â9. https://doi.org/10.2337/ds17-0045PMID:29151714
21.Gonder-Frederick LA, Shepard JA, Grabman JH, Ritterband LM. Psychology, technology, and diabetes management. Am Psychol. 2016 Oct;71(7):577â89. https://doi.org/10.1037/a0040383PMID:27690486
22.HomaK,Detzer M, Morgan J, et al. Diabetes specialty clinic: an intervention to improve care for veterans. Qual Manag Health Care. 2013 Jan-Mar;22(1):66â82. https://doi.org/10.1097/QMH.0b013e31827decaaPMID:23271595
23.Mosely K, Aslam A, Speight J. Overcoming barriers to diabetes care: perceived communication issues of healthcare professionals attending a pilot Diabetes UK training programme. Diabetes Res Clin Pract. 2010 Feb;87(2):e11â4. https://doi.org/10.1016/j.diabres.2009.12.003PMID:20044163
24.Bateman J. Psychologists in diabetes care. Diabetes & Prim Care. 2018;20(4):161â4.