Ramadan: a practical approach for diabetes educators

Introduction
The holy month of Ramadan falls between Monday 12 April and Tuesday 11 May in 2021. The Islamic Council of Victoria highlights that although Islam is a single religion, Muslim people are not a single homogenous group, with more than 500,000 Muslims living in Australian from over 70 countries around the world. Fasting during Ramadan is one of the Five Pillars of Islam and is obligatory for all healthy Muslims who have reached puberty. Followers are required to refrain from eating or drinking between dawn and sunset, including taking oral medications and smoking. People with a chronic disease, those who are unwell, the elderly and women who are pregnant or breastfeeding are exempt from fasting, however many people with diabetes actively choose to fast.
In order to provide client-centred care, it is important for diabetes educators to understand the importance of fasting and the changes in diabetes management required to assist clients to safely fast. Depending on the year and geographic location, fasting can last between 11 and 19 hours.
Guidelines for diabetes management during Ramadan
Several clinical guidelines have been developed to support health care professionals working with people with diabetes who choose to fast during Ramadan.1-2 The International Diabetes Federation in collaboration with the Diabetes and Ramadan International Alliance (IDF-DAR) released a comprehensive document in 2016 titled Diabetes and Ramadan: Practical Guidelines and more recently a free on-line short course on the IDF website.1 This publication was ground breaking at the time, with its focus on risk stratification and clinical recommendations.
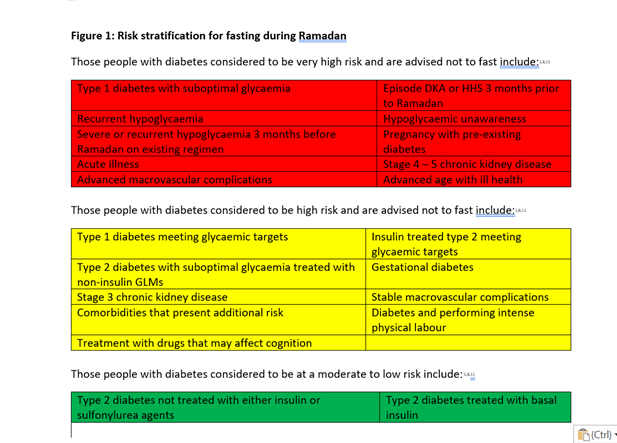
Using the IDF-DAR publication, the Australian Diabetes Society provides three practical resources: one for people with diabetes, one for Imams (Islamic leaders) and one for health care professionals (HCPs).3-5 Each brochure incorporates the IDF-DAR recommendations of risk stratification. This includes a traffic light approach whereby specific risks are highlighted to identify individuals with diabetes who are advised not to fast (red), those who may require additional support (amber) and those who could fast with minimal intervention (green) – see Figure 1.
The recently revised RACGP Management of type 2 diabetes: A Handbook for general practice, takes a slightly different approach.6 The American Diabetes Association and the European Association for the Study of Diabetes consensus report on the Management of Hyperglycaemia in Type 2 Diabetes, 2018, released a revised version last year focusing solely on the decision cycle of clinical care, education, nutrition and modifications with respect to all glucose lowering medicines (GLM) during Ramadan.2 With its two goals of care being to manage symptoms and prevent complications, this publication clearly outlines how each class of GLM could be used, modified or ceased during Ramadan.
Regardless of which set of clinical guidelines are used, assessment and structured education is required. The time preceding Ramadan is an ideal opportunity for diabetes educators to educate and work with their clients to plan for this important event. The most important thing to do as diabetes educators is to simply ask if our clients are planning to fast for Ramadan. It is also essential that we support individual choice and can provide management strategies to assist in fasting and that we are aware of available resources and undertake the upskilling required to support our clients. Being open and receptive is extremely important as seen in a qualitative study conducted in Melbourne in 2014 which found that women with Gestational Diabetes (including those requiring insulin) often chose to hide their fasting from HCPs.7
In the UK a whole systems approach known as ‘A Safer Ramadan’ was undertaken several years ago.8 The three arms to this intervention focused on raising community awareness of the impact of Ramadan and diabetes including the production of a slide set designed to be delivered by local community leaders and HCPs to reach a wide range of audiences. The second element was the development and delivery of HCP training module. The final component was a three-hour group structured self-management education program for people with diabetes promoting informed choices around fasting and supported with interactive resources. This paper may be useful for health professionals who are looking to do something similar within their own facility or community.
Managing risks – the importance of assessment and education
Fasting during Ramadan increases the risks for hyperglycaemia, Diabetic Ketoacidosis, dehydration and thrombosis.1 It should be noted that up to 30% of Muslims fast intermittently throughout the year.1
However, the main concern for diabetes management during Ramadan is hypoglycaemia and individuals receiving pre-Ramadan education experience less hypoglycaemia. 9 There are a number of factors, in addition to the propensity for hypoglycaemia, to consider for risk stratification including:10
- Type of diabetes
- Current diabetes treatment
- Degree of diabetes management
- Competence at self-management
- Previous Ramadan experience
- Presence of diabetes-related complications
- Presence of other co-morbidities
- Ongoing or recent intercurrent illness
- Degree of frailty
- Level of cognition
- Polypharmacy burden
- Occupation
- Social circumstances
In a study conducted over 12 clinics in four Middle Eastern countries, 515 people with type 2 diabetes received individualised education prior to Ramadan, self-management activities such as increased frequency of blood glucose monitoring, changes to diet and exercise were more likely to be undertaken compared to 259 clients who received usual care.11 Eighty percent of participants increased the frequency of their blood glucose monitoring during Ramadan. Both cohorts had similar symptom reporting of mild hypoglycaemia and hyperglycaemia, though a higher rate of moderate hypoglycaemia was seen in the intervention group. Participants receiving pre-Ramadan education were less likely to experience severe hypoglycaemia requiring medical assistance or hospitalisation for any other reason. Of note the intervention group lost on average nearly 3kg during the month of Ramadan compared to 0.5kg weight loss for the control group.
All clinical guidelines focus on the importance of pre-Ramadan assessment, as a number of key diabetes self-management issues will require review and possibly revision to meet the two goals of care: management of symptoms and prevention of complications. Assessment and education should include:
- Self-monitoring of blood glucose, not just the frequency which may be increased, but also that it is allowed to be undertaken during the day
- Dietitian review and education that focuses on how to break the fast (maximum of 3 dates), carbohydrate intake, minimising foods high in refined sugar and saturated fats, portion control, increased fluid intake especially with the pre-dawn meal of Suhoor, and the types of drinks consumed (avoiding caffeinated and sweetened drinks)
- Physical activity including during Taraweeh at night, which can be a very active form of prayer
- Smoking invalidates a fast and is an ideal opportunity to promote smoking cessation
- Review of glucose lowering medicines, with particular focus on insulin and sulfonylureas, but also changing regimens and administration time to fit within non-fasting periods
- Review of other medicines such as diuretics
- When to break the fast in terms of low or raised blood glucose levels
- Sick day management plans
- Eid-ul-Fitr three-day festival post-Ramadan
People with diabetes considered at very high and high risk who wish to fast, should attempt a trial fast prior to Ramadan, especially if changes have been made to their medicine regimen to support fasting. Part of a person’s Diabetes Ramadan Plan may consist of having the occasional ‘day off’ from fasting, rather than undertake the continuous 30-day period, which could be made up later in the year, however there appears to be some variation in opinion as to whether and how this can be undertaken among different communities. As we move into more hours of daylight in Australia each year during Ramadan (commencing 2nd April 2022 and 22nd March 2023), this may pose additional challenges to people with complex medical conditions. If fasting days could not be undertaken outside Ramadan, a redemption fee of ‘fidyah’ can be made. Diabetes complications screening should be completed prior to Ramadan or be booked in directly after Ramadan, as Muslims with diabetes often are uncomfortable to undertake pathology testing at this time. Sick day management and sick day plans should also be updated, especially for those clients taking sodium-glucose cotransporter-2 inhibitors. 12
Technologies such as continuous glucose and flash glucose monitoring, which have illustrated significant glucose variability in those taking part in Ramadan may assist people with diabetes to reduce variability and hypoglycaemia during fasting.13
Medication adjustments during Ramadan
Current guidelines recommend that the decision to start any new GLMs should be implemented and assessed before Ramadan and that communication be open to review and adjust GLMs especially if hypoglycaemia or medicine intolerability occurs during fasting.2
Recommended changes to common non-insulin glucose lowering medicines2, 6, 12
| Prior to Ramadan | During Ramadan |
| Metformin | No change in total daily dose Once a day – usual dose at Iftaar (evening) meal Twice a day – usual dose at Iftaar and Suhoor Three times a day – combine lunch dose with Iftaar, |
| Sulfonylurea | Consider either substituting, stopping or reducing dose |
| SGLT2i | No change in dose – should be well established prior to Ramadan Ensure adequate hydration, take with Iftaar Do not commence immediately prior or during Ramadan |
| GLP1RA | No change in dose – should be well established prior to Ramadan (8 weeks) Reduce or stop if nausea or vomiting occurs |
| DPP4i | No change in total daily dose |
Recommended changes to insulin for people with type 2 diabetes2, 14
| Insulin therapy | Dosing advice |
| Basal insulin | Once daily dosing administered in evening, may need dose reduction 15-30% Twice daily dosing – reduce morning dose at Suhoor by 25-50% |
| Bolus insulin | Omit lunchtime dose May require increased dose with Iftaar Reduce morning dose at Suhoor by 25-50% |
| Premixed insulin | Higher risk for hypoglycaemia on bd dosing Usually take normal dose with Iftaar Reduce morning dose at Suhoor by 25-50% May consider switching to basal insulin for Ramadan |
| Co-formulated insulin | Currently no recommendation Likely no change to daily dosing taken with Iftaar BD dosing – consider reducing dose at Suhoor by 25-50% |
Ibrahim et al (2020) recommend using a basal insulin known to have a lower risk of hypoglycaemia such as U300 glargine.2 In a trial of 263 adults in five countries with type 2 diabetes, Ryzodeg70/30® reduced severe and nocturnal hypoglycaemic events in participants fasting during Ramdan compared to Novomix30®.13 However the longer half-life of both Toujeo® (U300 glargine) and Ryzodeg70/30® must be considered and changes to dosing incorporated two to three days prior to the commencement of Ramadan. Ibrahim et al (2020) has also produced an algorithm for premixed insulin titration during Ramadan for people with type 2 diabetes, below.
| Fasting/pre-meal blood glucose | Recommended action |
| >16.6mmol/L | Break the fast Increase daily insulin dose by 20% |
| >10mmol/L | Increase insulin daily dose by 10% |
| 5.5 – 10.0mmol/L | No change |
| <3.9mmol/L | Break the fast Reduce insulin daily dose by 20% |
| <2.8mmol/L | Break the fast Stop insulin – OR reduce insulin daily dose by 30-40% |
Conclusion
Every year many Muslims with diabetes will fast during Ramadan. Unfortunately some HCPs may fail to appreciate the significance of this time and the religious and cultural sensitivities involved. This can mean that our clients may not be telling us the truth about fasting and may struggle to self-manage their diabetes without professional input, impacting on both their quality of life and safety. Asking the question, starting the conversation, increasing our awareness of Ramadan and becoming familiar with the consensus guidelines to better manage diabetes are some of the most important things we can offer to our Muslim clients.
Acknowledgements
Resources:
Australian Diabetes Society
- Diabetes during Ramadan: Patient Guide – PDF https://diabetessociety.com.au/documents/DARPatientLeaflet-Copy.pdf
- Ramadan and Diabetes: Guidance Sheet for Imam – PDF https://diabetessociety.com.au/documents/DARImamleaflet-Copy.pdf
- Management of Diabetes During Ramadan: Quick Reference Guide for Health Professionals – PDF https://diabetessociety.com.au/documents/DARHCPLeaflet-Copy.pdf
Diabetes NSW & ACT (2019)
- Managing diabetes during Ramadan May 2019 https://diabetesnsw.com.au/about-us/blog/managing-diabetes-during-ramadan/
Diabetes UK (2017)
- Fasting and managing your diabetes during Ramadan: English https://www.diabetes.org.uk/resources-s3/2017-09/1118A_Ramadan%20Factsheet_Update_April2017_amended.pdf
- Fasting and managing your diabetes during Ramadan: Arabic https://www.diabetes.org.uk/resources-s3/2017-09/Ramadan%20Factsheet_to%20send%20-%20Arabic.pdf
- Fasting and managing your diabetes during Ramadan: Bengali https://www.diabetes.org.uk/resources-s3/2017-09/Ramadan%20Factsheet_to%20send%20-%20Bengali.pdf
Fasting and managing your diabetes during Ramadan: Urdu https://www.diabetes.org.uk/resources-s3/2017-09/Ramadan%20Factsheet_to%20send%20-%20Urdu.pdf
References
1.The International Diabetes Federation in collaboration with the Diabetes and Ramadan International Alliance (IDF-DAR) released a comprehensive document in 2016 titled Diabetes and Ramadan: Practical Guidelines April 2016.
2.Ibrahim. M, Davies. M, Ahmad. E et al Recommendations for management of diabetes during Ramadan: update 2020, applying the principles of the ADA/EASD consensus. BMJ Open Diab Res Care 2020;8:e001248.Â
3.Australian Diabetes Society Diabetes during Ramadan: Patient Guide https://diabetessociety.com.au/documents/DARPatientLeaflet-Copy.pdfÂ
4.
Australian Diabetes Society Ramadan and Diabetes: Guidance Sheet for Imam https://diabetessociety.com.au/documents/DARImamleaflet-Copy.pdfÂ
5.
Australian Diabetes Society Management of Diabetes During Ramadan: Quick Reference Guide for Health Professionals https://diabetessociety.com.au/documents/DARHCPLeaflet-Copy.pdfÂ
6.
Royal Australian College of General Practitioners Management of type 2 diabetes: A handbook for general practice. East Melbourne July 2020.Â
7.
Ritchie. A, Robins. M, Hutchinson. A, Varadarajan. S, Howat. P Qualitative study: Perceptions of women with previous gestational diabetes during Ramadan pertaining to fasting. Presented at the ADIPS Conference 2015, Gold Coast.Â
8.
Daly. H, Byrne. J, Martin-Stacey. L et al âA Safer Ramadanâ: developing an integrated approach to support safer fasting and feasting for people with type 2 diabetes. Practical Diabetes 2014;31:292-7.Â
9.
Yorke. E, Atiase. Y Impact of structured education on glucose control and hypoglycaemia in type-2 diabetes: a systematic review of randomized controlled trials Ghana Med J 2018;52:41-60.Â
10.
Ahmed. S, Chowdhury. T, Hussain. S et al Ramadan and Diabetes: A Narrative Review and Practice Update Diabetes The 2020 11:2477-2520.Â
11.
McEwan. L, Ibrahim. M, Ali. N et al Impact on an individualized type 2 diabetes education program on clinical outcomes during Ramadan BMJ Open Diab Res Care 2015;3:3000111.
12.
Grajower. M, Horne. B Clinical management of intermittent fasting in patients with diabetes mellitus Nutrients 2019;11:E873.
13.
Lessan. N, Hannoun. Z, Hasan. H et al Glucose excursion and glycaemic control during Ramadan fasting in diabetic patients: insights from continuous glucose monitoring (CGM) Diabetes Metab 2015;41:28-36. Â
14.
Hassanein. M Echtay. A, Malek. R et al Efficacy and safety of insulin degludec/insulin aspart in adults with type 2 diabetes fasting during Ramadan. Presented at the IDF Congress 2017, Abu Dhabi.